Idiopathic Intracranial Hypertension (IIH)
Overview
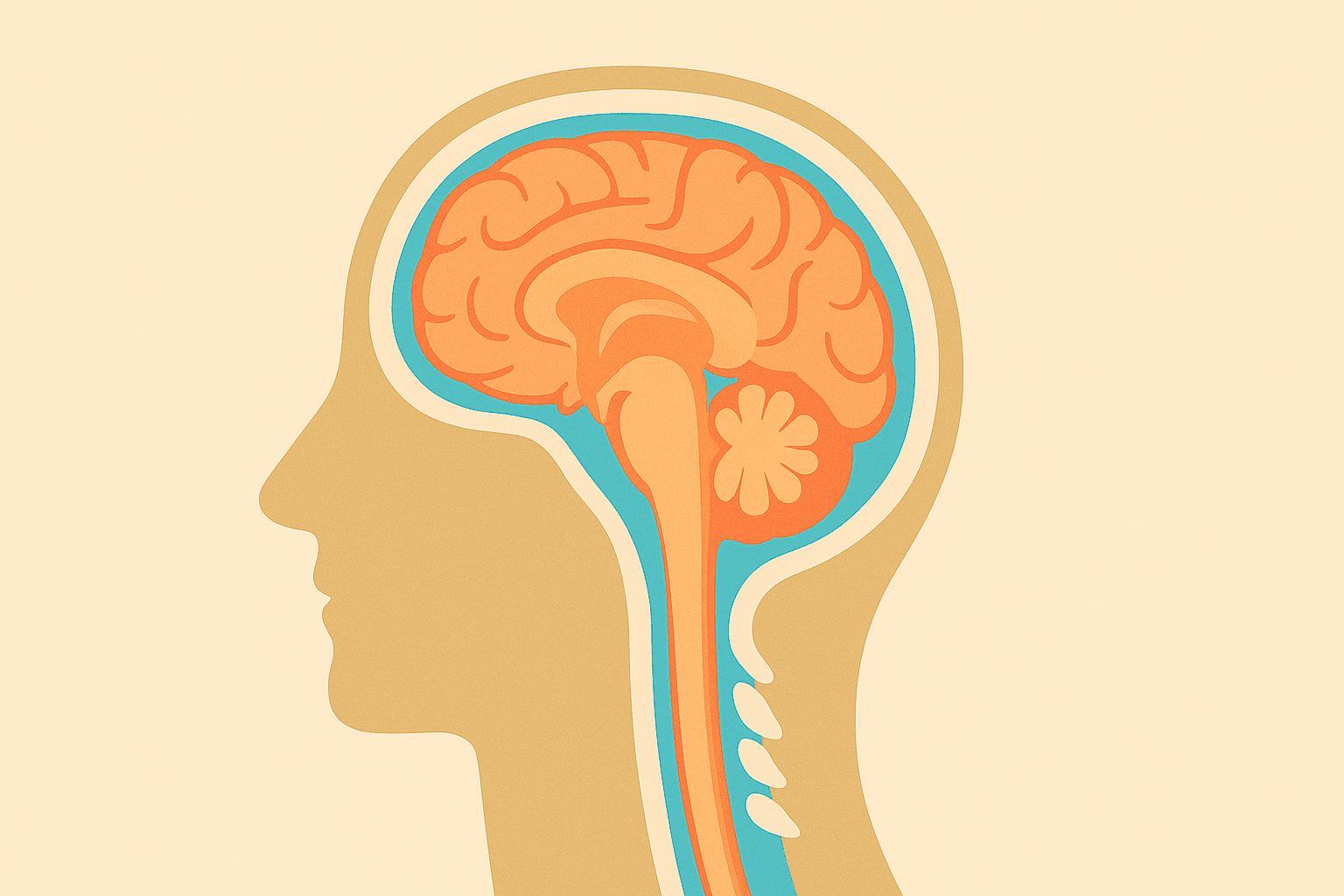
Idiopathic Intracranial Hypertension (IIH), also known as pseudotumour cerebri, is a condition where pressure builds up inside the skull without an obvious cause. This affects the cerebrospinal fluid that surrounds and protects the brain and spinal cord.

Common Symptoms
Headaches are the most frequent symptom, affecting up to 90% of people with IIH. These headaches are often:
- Severe and throbbing
- Worse in the morning or when lying down
- May worsen with coughing, sneezing, or straining
- Often described as feeling like pressure behind the eyes
Visual disturbances occur in about 70% of patients and may include:
- Blurred or double vision
- Brief episodes of vision loss (lasting seconds)
- Difficulty seeing to the sides (peripheral vision loss)
- Seeing flashing lights or "sparkles"
Pulsatile tinnitus - hearing a whooshing or pulsing sound in one or both ears that matches your heartbeat - affects about 60% of people with IIH.
Less Common Symptoms
- Nausea and vomiting
- Dizziness or balance problems
- Neck and shoulder pain
- Memory problems or difficulty concentrating
- Fatigue
Warning Signs
Some symptoms require immediate medical attention:
- Sudden, severe vision loss
- Rapid worsening of headaches
- New weakness or numbness
Primary Risk Factors
Being overweight or obese is the strongest risk factor, particularly for women. About 90% of women with IIH are significantly overweight. The connection isn't fully understood, but may relate to how excess weight affects hormones and fluid pressure in the body.
Gender and age play important roles. IIH is 8-10 times more common in women than men, particularly women of childbearing age (20-40 years). This suggests hormonal factors may be involved. In men, the condition is less commonly associated with weight, but may be linked to obstructive sleep apnoea and low testosterone levels.
Recent weight gain can trigger IIH, even in people who aren't significantly overweight overall.
Secondary Factors
Certain medications have been associated with IIH, including:
- Some antibiotics (particularly tetracyclines such as doxycycline and minocycline)
- Vitamin A supplements (in high doses - small doses in multivitamin preparations are unlikely to cause issues unless taken for extended periods)
- Some acne medications
- Certain steroids
Medical conditions that may increase risk include:
- Sleep apnoea
- Polycystic ovary syndrome (PCOS)
- Kidney disease
- Some autoimmune conditions
Hormonal changes such as starting oral contraceptives may trigger symptoms in susceptible individuals.
Diagnosis
Diagnosing IIH requires a systematic approach to rule out other causes of increased brain pressure and confirm the characteristic features of the condition.
Initial Assessment
Medical history and examination: Your neurologist will ask detailed questions about your symptoms, medications, and medical history. A thorough neurological examination checks for signs of increased pressure and any other neurological problems.
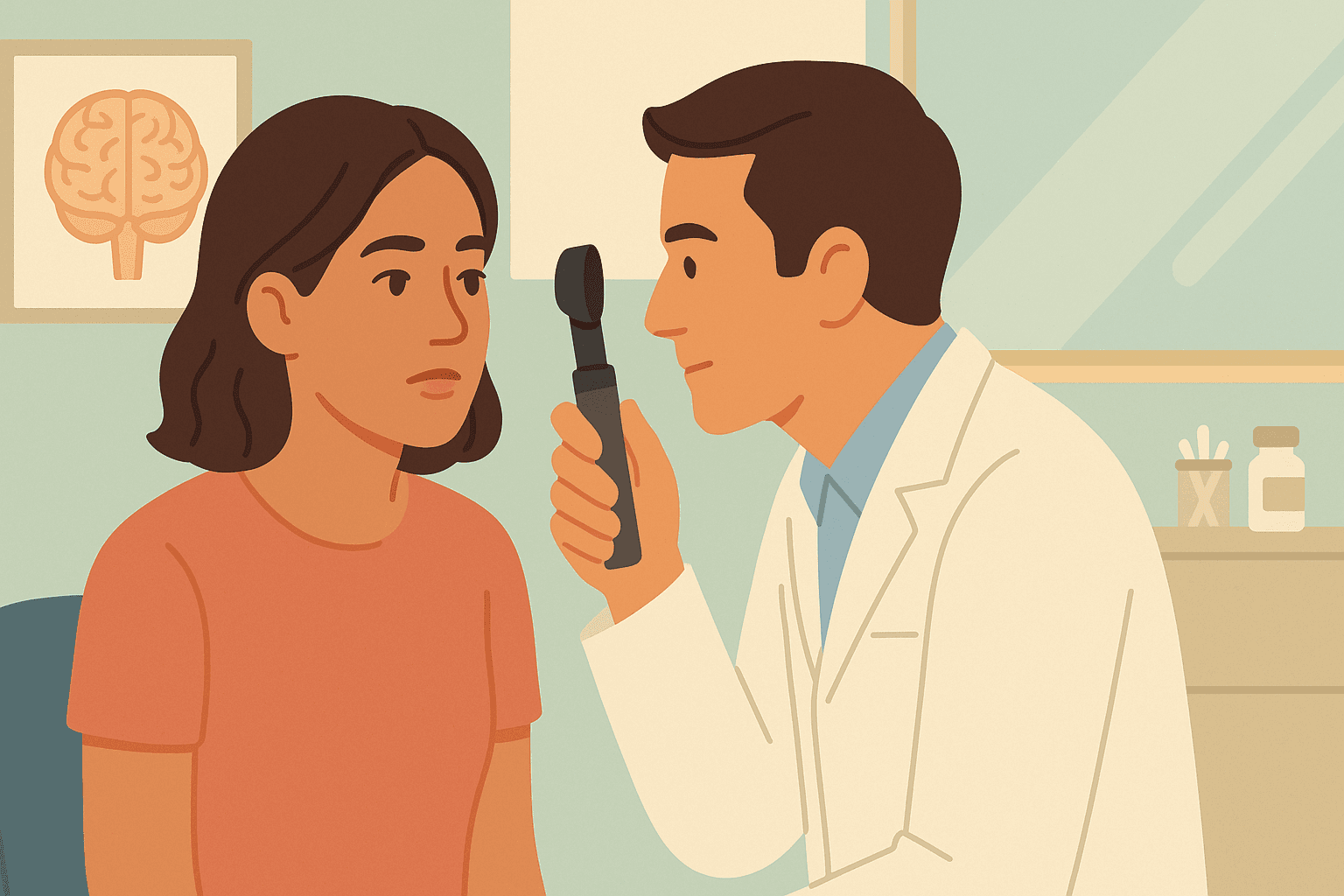
Eye examination: A comprehensive eye exam is essential and can be performed by an ophthalmologist, optometrist, or even a neurologist using specialised equipment. If you've recently seen an optometrist, this is often sufficient to detect any abnormalities. The examination will look for:
- Papilloedema (swelling of the optic nerve)
- Changes in visual fields
- Any vision loss
Imaging Studies
MRI of the brain is performed to:
- Rule out brain tumours, blood clots, or other structural problems
- Look for signs consistent with increased pressure
- Check the brain's venous drainage system
MR venography should ideally be included as part of the MRI scanning protocol when IIH is suspected, as it examines the brain's drainage vessels in detail. If the initial MRI was performed for non-specific symptoms like headache and didn't include this sequence, patients may need a repeat MRI to properly assess the venous drainage system.
Lumbar Puncture (Spinal Tap)
This is the definitive test for IIH. A thin needle is inserted into the lower back to:
- Measure the pressure of cerebrospinal fluid
- Collect fluid for analysis to rule out infections
- Sometimes provide temporary symptom relief
The procedure is performed under local anaesthetic and usually takes about 5-10 minutes. If headaches are pressure-driven, some people experience relief immediately after the procedure. However, if headaches are migrainous or from other causes, they may not improve or could even worsen. Post-lumbar puncture headache is a common complication that can occur after the procedure.
Additional Tests
Visual field testing maps your complete field of vision to detect any areas of vision loss. Abnormalities detected on visual field testing are serious and should trigger an urgent appointment with either a neurologist or ophthalmologist. If you are seeing an optometrist, ensure that they check this for you.
OCT (Optical Coherence Tomography) is the most accurate way to detect and measure swelling of the optic nerve and retina that may be associated with raised intracranial pressure. Besides monitoring symptoms, OCT provides the most objective way to track progress and treatment response over time.
Understanding Headaches in IIH
Headaches are the most common and often most debilitating symptom of IIH, but it's important to understand that not all headaches in IIH patients are the same. This complexity is why specialised neurological care is often essential for optimal headache management.
Types of Headaches in IIH
Pressure-related headaches are directly caused by the increased intracranial pressure. These headaches typically:
- Worsen when lying down or bending over
- Improve when standing upright
- May be relieved by treatments that reduce brain pressure
- Often feel like severe pressure behind the eyes or throughout the head
Secondary headaches can develop as a result of IIH but have different underlying mechanisms:
- Migraine headaches may be triggered or worsened by the stress of having IIH
- Occipital headaches arise from tension in the muscles at the base of the skull
- Cervicogenic headaches originate from neck problems that can develop due to altered posture or muscle tension
Why Specialised Care Matters
Whilst reducing intracranial pressure often helps with many types of headaches in IIH, it may not completely resolve all headache types. Effective headache management frequently requires:
- Targeted therapies for specific headache types (migraine medications, muscle relaxants, nerve blocks)
- Combination approaches that address both pressure and secondary headache mechanisms
- Ongoing adjustment of treatments based on response and changing symptoms
This is why involvement of a neurologist experienced with IIH disorders is often important. They can distinguish between different headache types and develop comprehensive treatment plans that address all contributing factors, not just the elevated pressure.
What This Means for Patients
Understanding that your headaches may have multiple causes can be reassuring - it explains why pressure-reducing treatments alone might not completely eliminate all headaches, and why additional targeted therapies may be necessary for complete headache remission.
Treatment Options
Treatment for IIH aims to reduce the pressure inside the skull, relieve symptoms, and most importantly, protect vision. The approach is tailored to each individual based on their symptoms, degree of vision problems, and personal circumstances.
It's important to note that whilst weight loss may improve the condition in obese patients, it may not result in complete cure of the disease in up to 30% of cases. This is because a significant proportion of patients have secondary IIH or IIH caused by non-hormonal or non-obesity related disorders. However, weight loss is recommended for all patients who are above a normal body mass index.
Lifestyle Modifications
Weight loss is often the most effective treatment for overweight patients. Even modest weight loss (5-10% of body weight) can lead to significant improvement in symptoms and pressure reduction. This works best when combined with dietary guidance and supervised exercise programs.
Dietary changes may include reducing salt intake and staying well-hydrated. Some patients benefit from working with a dietitian.
Medications
Acetazolamide is the most commonly prescribed medication for IIH. It works by reducing the production of cerebrospinal fluid, thereby lowering pressure. Most patients start with a low dose that's gradually increased based on response and tolerance.
Topiramate is an alternative medication that can also help reduce fluid production and may assist with weight loss as a side effect.
Diuretics (water tablets) are sometimes used, though they're generally less effective than acetazolamide.
Procedures
Repeated lumbar punctures may provide temporary relief whilst other treatments take effect. These are typically used sparingly due to patient comfort considerations.
Choosing the Right Procedure
The choice of procedure depends on several factors including the severity of symptoms, degree of vision threat, and underlying anatomy. Transverse sinus stenting is typically considered when MR venography shows significant narrowing of the brain's drainage vessels and may be preferred in younger patients or those wanting to avoid more invasive surgery. Optic nerve sheath fenestration is specifically chosen when vision is rapidly deteriorating and the primary goal is to protect sight, though it may not improve headaches. CSF shunting is generally reserved for cases with severe, persistent symptoms that don't respond to medications and other procedures, particularly when both headaches and vision problems need to be addressed. The decision is individualised based on each patient's specific circumstances and requires careful discussion between patient and specialist.
Understanding Procedure Risks and Complications
Each surgical intervention carries specific risks and potential complications that patients should understand when making treatment decisions.
Transverse Sinus Stenting Risks: Generally considered the safest option with serious complications occurring in 1-2% of cases. Most patients experience temporary headache on the side of the stent placement. Rare but serious complications include bleeding around the brain. The long-term effects of having a permanent stent are still being studied, particularly in younger patients.
Optic Nerve Sheath Fenestration Risks: This procedure has a good safety profile for serious complications, but treatment failure rates are significant. About one-third of patients may experience worsening vision again within 1-3 years, requiring repeat procedures. While effective for protecting vision, it's less successful for treating headaches. Minor complications include temporary eye swelling and irritation.
CSF Shunting Risks: Shunting procedures have the highest complication and failure rates among IIH treatments. Many patients require multiple revision surgeries over time. Common problems include shunt blockage, infection, over-drainage, and catheter movement. Lumboperitoneal shunts may cause additional complications like spinal problems, whilst ventriculoperitoneal shunts generally have lower complication rates but still require ongoing monitoring.
Transverse sinus stenting is a newer procedure where a small tube (stent) is placed in the brain's venous drainage system to improve blood flow and reduce pressure. This may be considered when there is evidence of venous narrowing contributing to the condition.
Optic nerve sheath fenestration is a microsurgical procedure that creates a small opening around the optic nerve to relieve pressure. This is considered when vision is threatened and medications aren't sufficient.
CSF shunting involves placing a tube to drain excess cerebrospinal fluid from around the brain to another part of the body (usually the abdomen). This is typically reserved for severe cases that don't respond to other treatments.
Monitoring and Follow-up
Regular monitoring is essential and typically includes:
- Periodic eye examinations and visual field tests
- Assessment of symptoms and medication tolerance
- Weight monitoring
- Repeat imaging when necessary
Your Healthcare Team: Specialists involved in IIH Care.
Managing IIH effectively often requires a multidisciplinary approach involving several specialists, each bringing unique expertise to your care.
Neurologist
Neurologists are often the primary specialists managing IIH. They coordinate your overall care, prescribe and monitor medications like acetazolamide, manage complex headache patterns, and make decisions about when additional treatments or procedures may be needed. Neurologists experienced with IIH disorders are particularly valuable for managing the multiple types of headaches that can occur.
Ophthalmologist or Neuro-ophthalmologist
Eye specialists play a crucial role in monitoring and protecting your vision. They perform detailed eye examinations, visual field testing, and OCT scans to track papilloedema and detect any vision changes. Neuro-ophthalmologists have additional training in conditions affecting both the eyes and nervous system, making them particularly skilled in IIH management.
Neurosurgeon
Neurosurgeons become involved when surgical intervention is needed, such as CSF shunting procedures. They assess whether surgery is appropriate, perform shunt operations, and manage any surgical complications. Their expertise is essential for the more invasive treatment options.
Interventional Neuroradiologist/Neurologist/Neurosurgeon
These specialists perform transverse sinus stenting procedures. They have expertise in navigating the brain's blood vessels and placing stents safely. They work closely with neurologists to determine which patients are candidates for stenting based on imaging findings.
Optometrist
Optometrists can perform initial eye examinations and visual field testing, often serving as the first point of detection for papilloedema. They play an important role in ongoing monitoring, particularly if you've recently had an eye examination when IIH is suspected.
Endocrinologist
An endocrinologist may be involved if there are hormonal factors contributing to your IIH, such as thyroid disorders or other endocrine conditions that might be related to your symptoms.
Gynaecologist or Clinical Reproductive Endocrinologist (CREI)
These specialists may be consulted if PCOS is thought to play a significant role in your condition, helping to manage hormonal factors that could be contributing to IIH.
Dietitian
For patients where weight management is important, dietitians provide specialised guidance on sustainable weight loss strategies and nutritional management, which can be crucial for long-term IIH control.
Your Role in the Team
You are the most important member of your healthcare team. Keeping track of your symptoms, adhering to treatments, attending regular follow-up appointments, and communicating changes in your condition ensures the best possible outcomes. Good communication between all team members, including you, is essential for successful IIH management.
When to Seek Urgent Medical Care
Whilst IIH is generally manageable with regular treatment, certain symptoms require immediate medical attention.
Emergency Symptoms
Sudden vision changes including:
- Rapid loss of vision in one or both eyes
- New or worsening double vision
- Sudden loss of peripheral vision
Severe headache changes such as:
- Sudden, severe headache unlike your usual pattern
- Headache with fever, rash, or neck stiffness
- Headache with confusion
Neurological symptoms including:
- New weakness or numbness in arms or legs
- Severe dizziness or balance problems
- Seizures
When to Contact Your Specialist
Gradual vision changes should be reported promptly even if not severe:
- Slowly progressive vision loss
- Increasing frequency of transient vision loss
- Changes in colour vision
Medication concerns including:
- Severe side effects from treatments
- Questions about medication effectiveness
- Need for dosage adjustments
Symptom changes such as:
- Worsening headache pattern
- New or worsening tinnitus
- Significant changes in symptoms despite treatment
Regular Monitoring Schedule
Most patients with IIH benefit from:
- Eye examinations every 3-6 months initially, then annually
- Neurological follow-up every 6-12 months
- More frequent monitoring if symptoms change or treatment is adjusted
Remember that IIH is a manageable condition when properly diagnosed and treated. Staying informed about your condition, maintaining regular medical follow-up, and promptly reporting any changes ensures the best possible outcomes.

Dr. Hugh Stephen Winters
Stroke and Interventional Neurologist, MBChB (Auckland), FRACP (Neurology), CCINR (Neurology)
Reviewed on: 22 May 2025



