Multiple Sclerosis
Overview
Multiple sclerosis (MS) is an autoimmune condition where your immune system mistakenly attacks the protective covering around nerve fibres in your brain and spinal cord. While there's no cure, effective treatments can slow disease progression and manage symptoms, allowing most people to live full, active lives.
What Is Multiple Sclerosis?
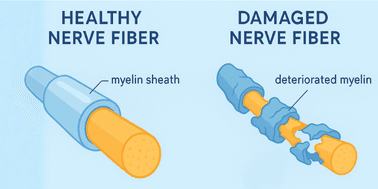
Multiple sclerosis is an autoimmune condition that affects your central nervous system—your brain, spinal cord, and optic nerves. Think of your nervous system like electrical wiring in your home. The nerve fibres are like the wires, and they're covered by a protective sheath called myelin, which acts like insulation around electrical cables.
In MS, your immune system mistakenly attacks this myelin covering. When the myelin is damaged:
- Nerve signals between your brain and body slow down or get blocked
- This causes various symptoms throughout your body
- The underlying nerve fibre may also become damaged over time
Key Facts:
- About 25,600 Australians live with MS
- It's twice as common in women and typically diagnosed between ages 20–40
- It's not contagious, directly inherited, or caused by anything you did wrong
- MS is treatable with modern medications that can significantly slow disease progression
What Causes Multiple Sclerosis?
The exact cause of MS isn't fully understood, but researchers believe it develops from a combination of factors:
Immune System Problems:
- Your immune system, which normally protects you from infections, mistakenly attacks your own nerve tissue
- This creates inflammation that damages the myelin
Environmental Factors:
- Previous Epstein-Barr virus (EBV) infection, low vitamin D levels, obesity, and cigarette smoking may increase risk
- Living further from the equator (like in southern Australia) slightly increases risk
- These factors may trigger MS in people who are already susceptible
Genetic Factors:
- MS isn't directly inherited, but having a family member with MS slightly increases your risk
- It's more about inheriting a susceptibility rather than the disease itself
Common Symptoms of Multiple Sclerosis
MS symptoms vary greatly from person to person. Symptoms vary widely among individuals and may include fatigue, numbness, muscle weakness, vision problems, and difficulty with coordination and balance.
Most Common Early Symptoms
Sensory Changes:
- Numbness or tingling, often in hands, feet, or face
- Areas of skin that feel different to touch
- Pain or unusual sensations
Vision Problems:
- Blurred or dimmed vision
- Pain when moving your eyes
- Temporary vision loss in one eye
Fatigue:
- Overwhelming tiredness that's different from normal tiredness
- Often the most challenging symptom to manage
- May worsen in heat or after physical activity
Muscle and Movement Issues:
- Weakness, often starting in the legs
- Muscle stiffness or spasms
- Balance problems or dizziness
- Coordination difficulties
Other Possible Symptoms
Cognitive Changes:
- Memory problems
- Difficulty concentrating
- Taking longer to process information
Bladder and Bowel Issues:
- Urgency or frequency
- Difficulty emptying the bladder completely
Mood Changes:
- Depression or anxiety (which are treatable)
- Emotional changes
Important Notes About Symptoms
- Heat sensitivity: Small increases in body temperature can temporarily worsen MS symptoms. These are known as pseudorelapses
- Symptoms come and go: Many people have periods where symptoms improve or disappear
- Everyone is different: You may have some, none, or different symptoms than what's listed here
- Symptoms alone don't diagnose MS: The symptoms described above are common in many conditions, not just MS. Having these symptoms doesn't mean you have MS, and not having them doesn't rule it out
- Imaging is crucial: MRI scans are often the most important factor in diagnosing MS, as they can show damage in your nervous system even when symptoms are mild or absent
- See a specialist: Only a neurologist can properly evaluate your symptoms and determine if further testing for MS is needed
Types of Multiple Sclerosis
There are three main types of MS: relapsing remitting MS (RRMS), secondary progressive MS (SPMS) and primary progressive MS (PPMS). Understanding the basic differences helps you communicate with your healthcare team.
Relapsing-Remitting MS (RRMS)
- Most common: An estimated 85% of people diagnosed with MS have this type
- Pattern: Symptoms appear suddenly (relapses), then improve or disappear (remission)
- Between relapses: You may feel completely normal or have mild ongoing symptoms
Primary Progressive MS (PPMS)
- Less common: Primary Progressive Multiple Sclerosis affects about 10-15% of people with MS
- Pattern: Symptoms gradually worsen over time without clear relapses
- Age: On average, people with primary-progressive MS start having symptoms between ages 35 and 39
Secondary Progressive MS (SPMS)
- Develops later: Secondary Progressive MS is a secondary phase of relapsing remitting MS that can develop years to decades following the initial onset of symptoms
- Good news: Modern treatments significantly reduce the risk of progression to SPMS
How Is Multiple Sclerosis Diagnosed?
There's no single test for MS. Diagnosing MS involves a combination of physical and neurological exams, along with various tests. Your doctor needs to see evidence of nerve damage in different parts of your nervous system occurring at different times.
The Diagnostic Process
Medical History:
- Your doctor will ask about your symptoms and when they started
- Family history of autoimmune conditions
- Previous illnesses or infections
Physical Examination:
- Testing your reflexes, strength, and coordination
- Checking your vision and eye movements
- Testing sensation and balance
MRI Scans:
- MRI is the gold standard imaging procedure for MS
- Shows areas of damage (lesions) in your brain and spinal cord
- May use contrast dye to show active inflammation
Other Tests (if needed):
- Blood tests to rule out other conditions
- Spinal fluid analysis (lumbar puncture)
- Tests of nerve function
What to Expect
Receiving an official MS diagnosis can take time and may require multiple visits to your provider. This is normal because:
- Symptoms may be subtle at first
- Your doctor needs to rule out other conditions
- Sometimes waiting for additional symptoms is necessary
Treatment Overview
The Good News: There are now several effective treatments that can help you manage the disease and live a long, full life.
Main Treatment Goals
Disease-Modifying Therapies (DMTs):
- Disease-modifying therapies (DMTs), such as interferon beta, glatiramer acetate, fingolimod, and ocrelizumab, can help reduce the frequency and severity of relapses and slow disease progression
- Work by reducing immune system attacks on myelin
- Most effective when started early
- Different options available as injections, tablets, or infusions
Symptom Management:
- Medications to help with specific symptoms like fatigue, pain, or muscle spasms
- Physical therapy to maintain strength and mobility
- Occupational therapy to help with daily activities
- Speech therapy if needed
Treatment Approach
Your neurologist will work with you to:
- Choose the right medication for your type of MS
- Monitor how well treatment is working
- Adjust treatment if needed
- Manage any side effects
- Address symptoms that affect your daily life
Living with Multiple Sclerosis
What This Means for Your Life
Many people with MS:
- Continue working and pursuing their careers
- Maintain active social lives and relationships
- Participate in sports and physical activities
- Travel and pursue hobbies
- Have families and raise children
Key Strategies:
- Take medications as prescribed
- Stay physically active within your abilities
- Eat a healthy, balanced diet
- Get enough rest and manage stress
- Stay connected with family and friends
- Work with your healthcare team regularly
Heat Management
Small increases in body temperature can temporarily worsen MS symptoms, so:
- Use air conditioning when possible
- Take cool showers or baths
- Drink cold fluids
- Plan outdoor activities for cooler times of day
- Consider cooling products like vests or towels
When to Seek Medical Help
See your doctor immediately if you experience:
- Sudden severe weakness
- Sudden vision loss
- Severe dizziness or loss of balance
- New symptoms that last more than 24 hours
- Significant worsening of existing symptoms
Regular follow-up care includes:
- Appointments with your neurologist every 3-6 months
- Annual MRI scans while on treatment
- Blood tests to monitor medication effects
- Allied health appointments as needed
Support and Resources
Healthcare Team
- Neurologist: Specialist doctor who diagnoses and treats MS
- MS nurse: Provides education and ongoing support
- General practitioner: Your regular doctor for overall health care
Australian Support Services
- MS Australia: National organisation providing information and support
- State MS societies: Local support groups and services
- NDIS: May provide funding for equipment and support services
Financial Considerations
- Most MS medications are covered under the PBS (Pharmaceutical Benefits Scheme)
- Medicare covers specialist consultations
- Private health insurance may reduce out-of-pocket costs
Key Takeaways
Remember:
- MS is a manageable condition with proper treatment
- Treatment can help manage MS and reduce the risk of disability
- Everyone's experience with MS is different
- Early treatment makes a significant difference
- You can live a full, active life with MS
- You're not alone—support is available
Next Steps:
- Learn about your specific type of MS
- Work closely with your neurologist to find the right treatment
- Connect with support services
- Focus on staying healthy overall
- Ask questions—your healthcare team is there to help
Questions to Ask Your Doctor:
- What type of MS do I have?
- What treatment options are available for me?
- How will we monitor my condition?
- What symptoms should I watch for?
- Where can I get additional support?

Dr. Hugh Stephen Winters
Stroke and Interventional Neurologist, MBChB (Auckland), FRACP (Neurology), CCINR (Neurology)
Reviewed on: 9 June 2025

